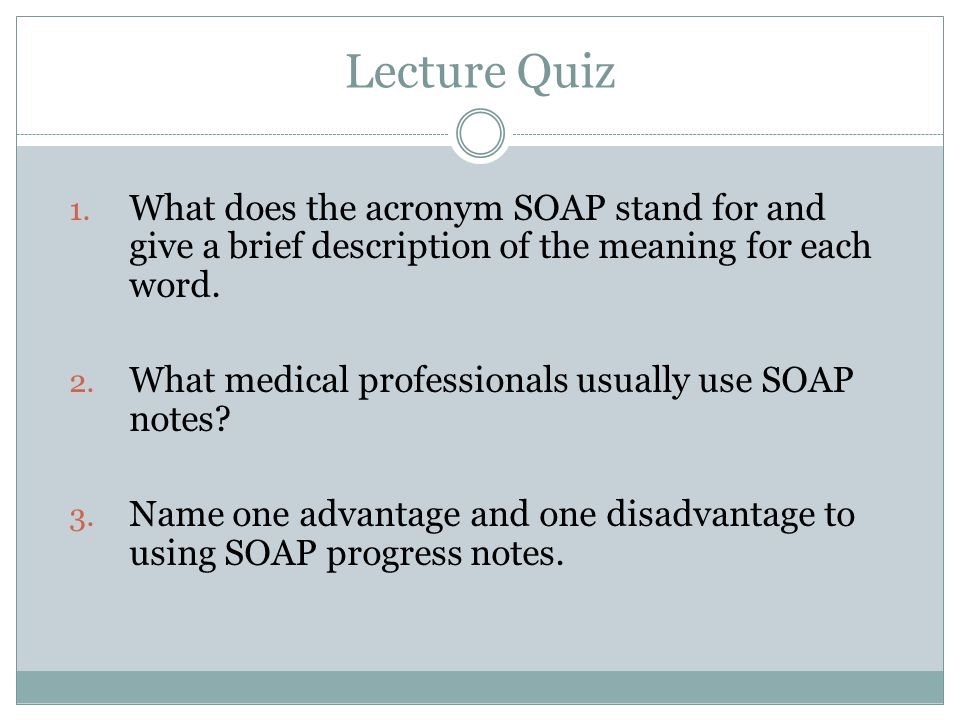
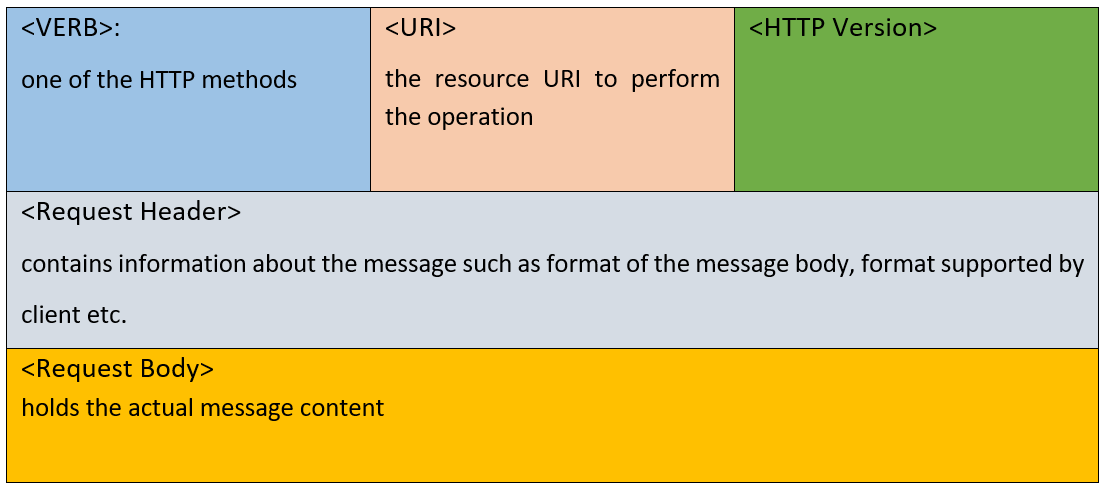
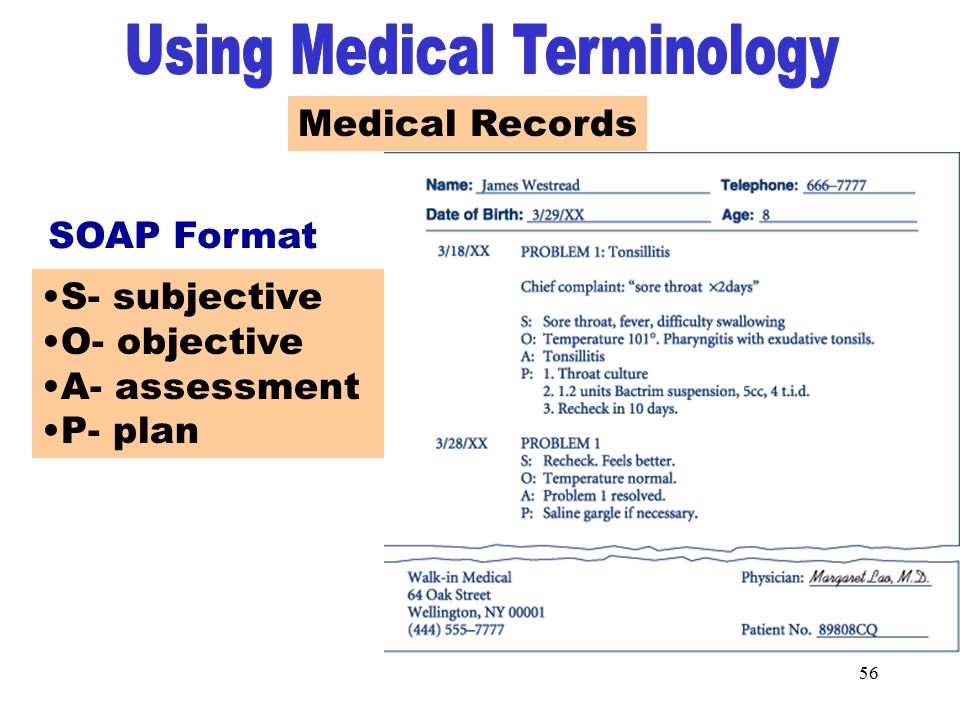
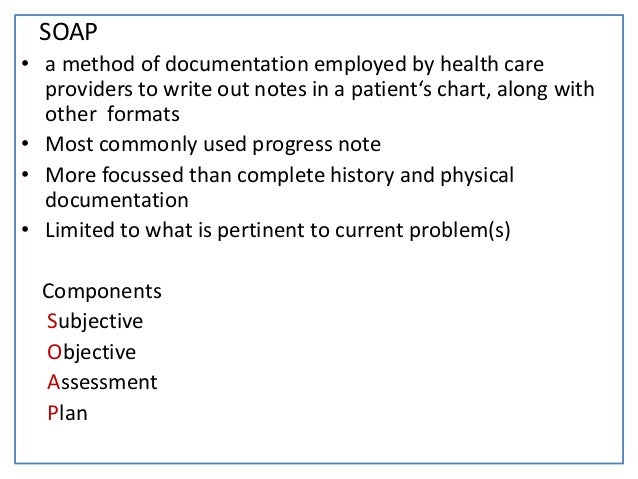
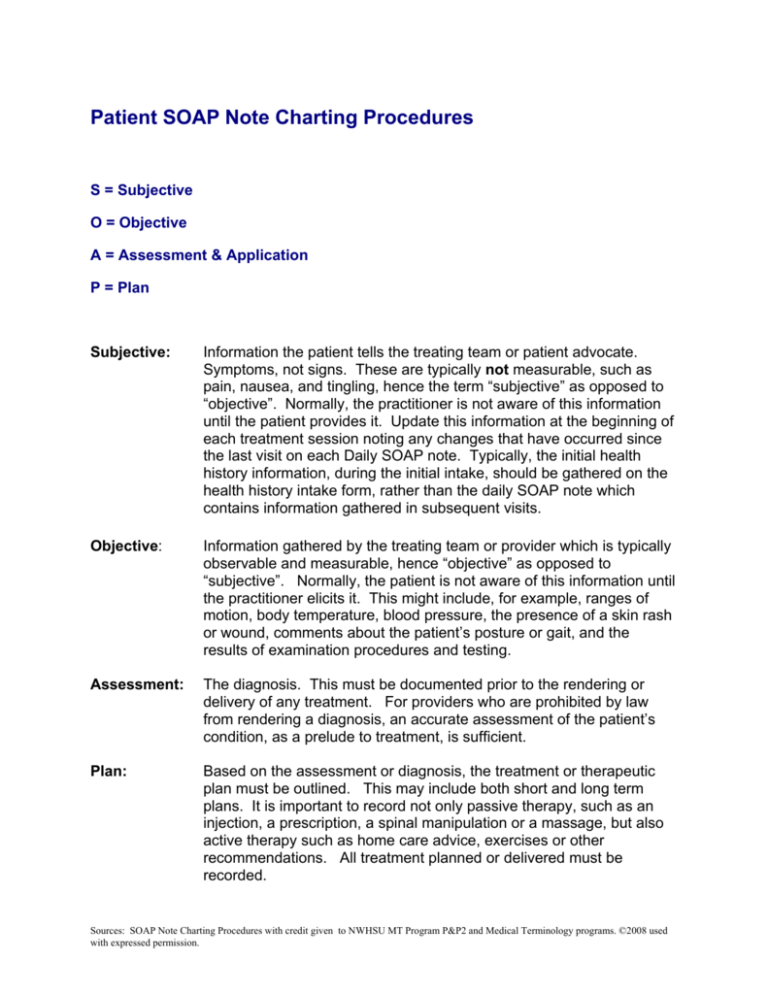
Find out what is the full meaning of SOAPER on Abbreviationscom!SOAP is an acronym that stands for subjective, objective, assessment and plan In this post, I'll discuss what information goes in each section of the SOAP note I also have some tips to help you write your SOAP notes faster and better The last section of this post talks about what you need to know about SOAP notes for the MBLExWhat does SOP abbreviation stand for?

Top 5 Skin Benefits Of Activated Charcoal Soap For Face
S.o.a.p meaning medical
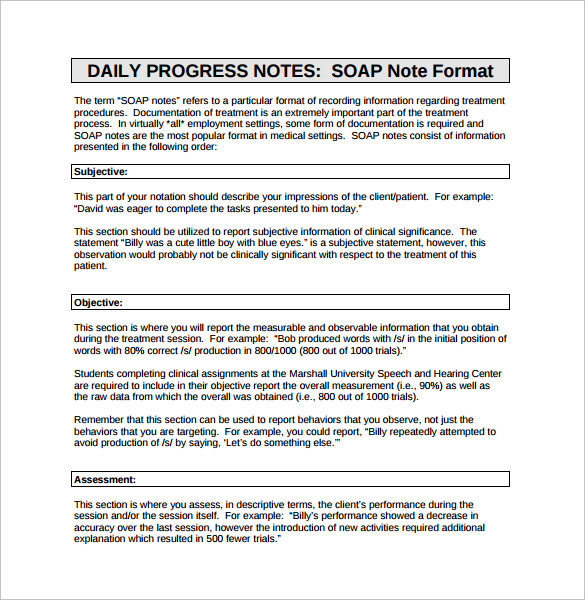
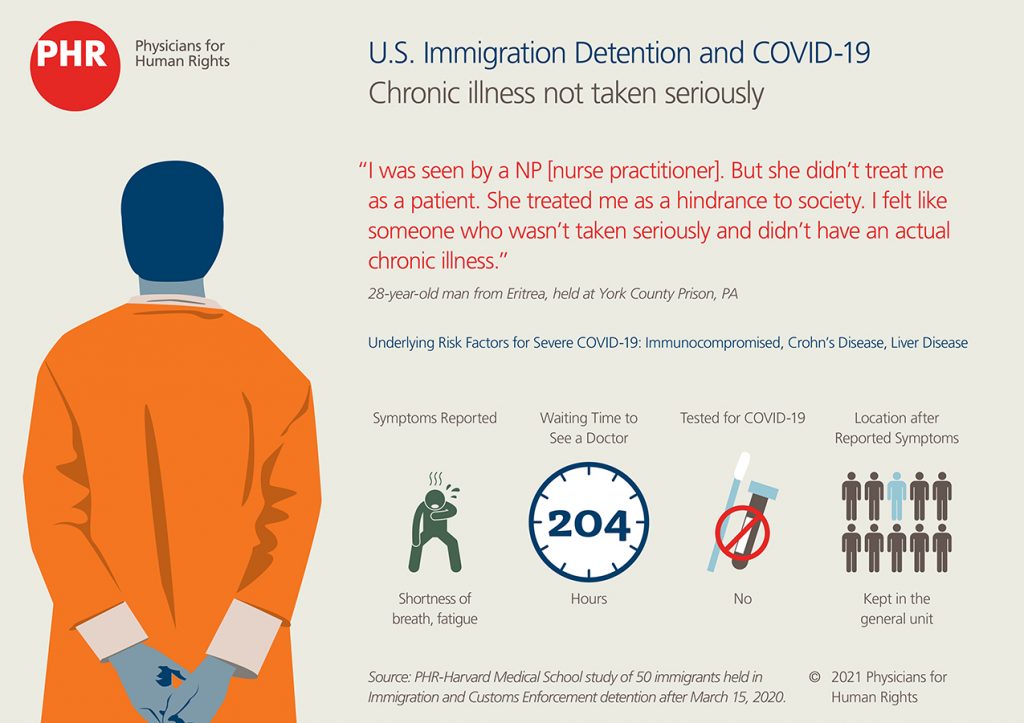
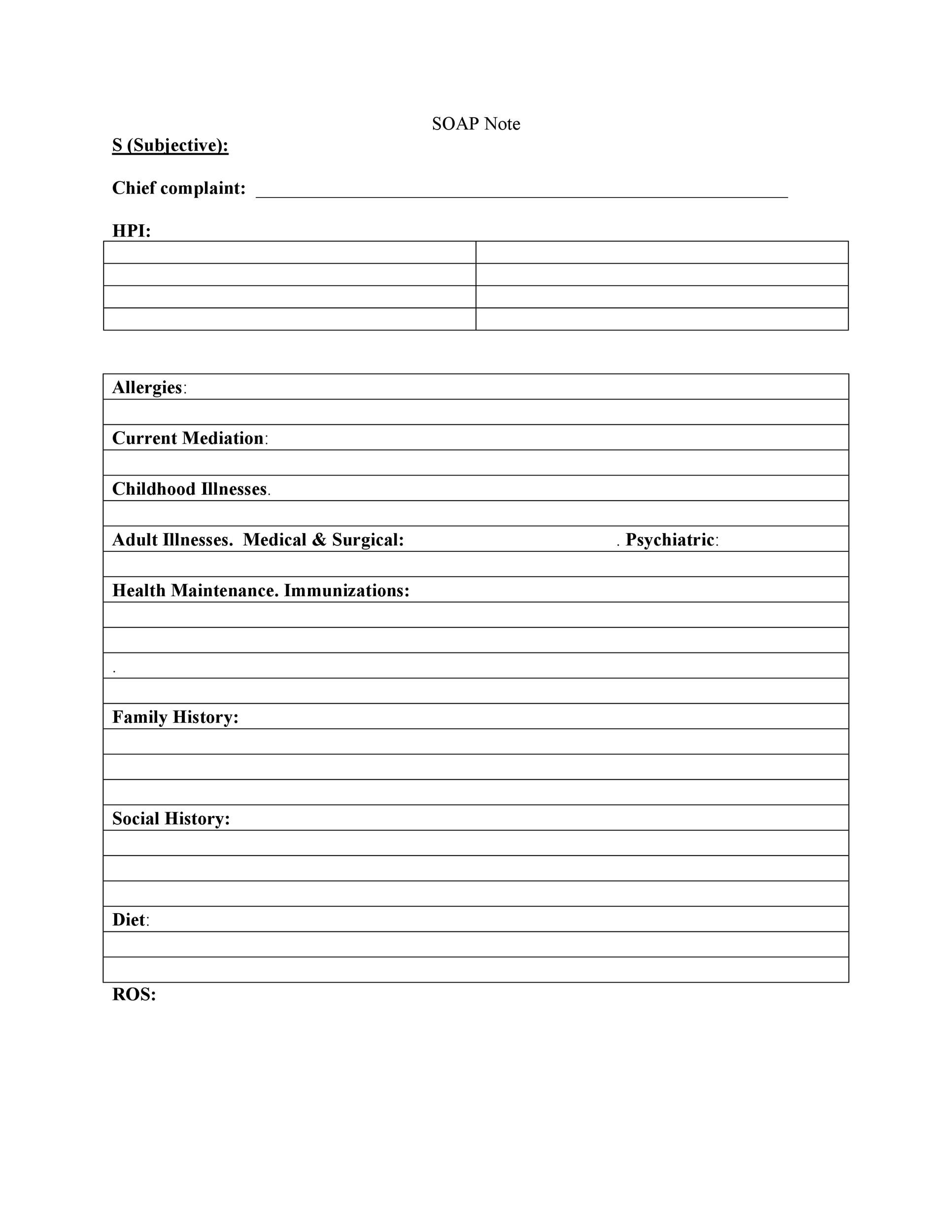
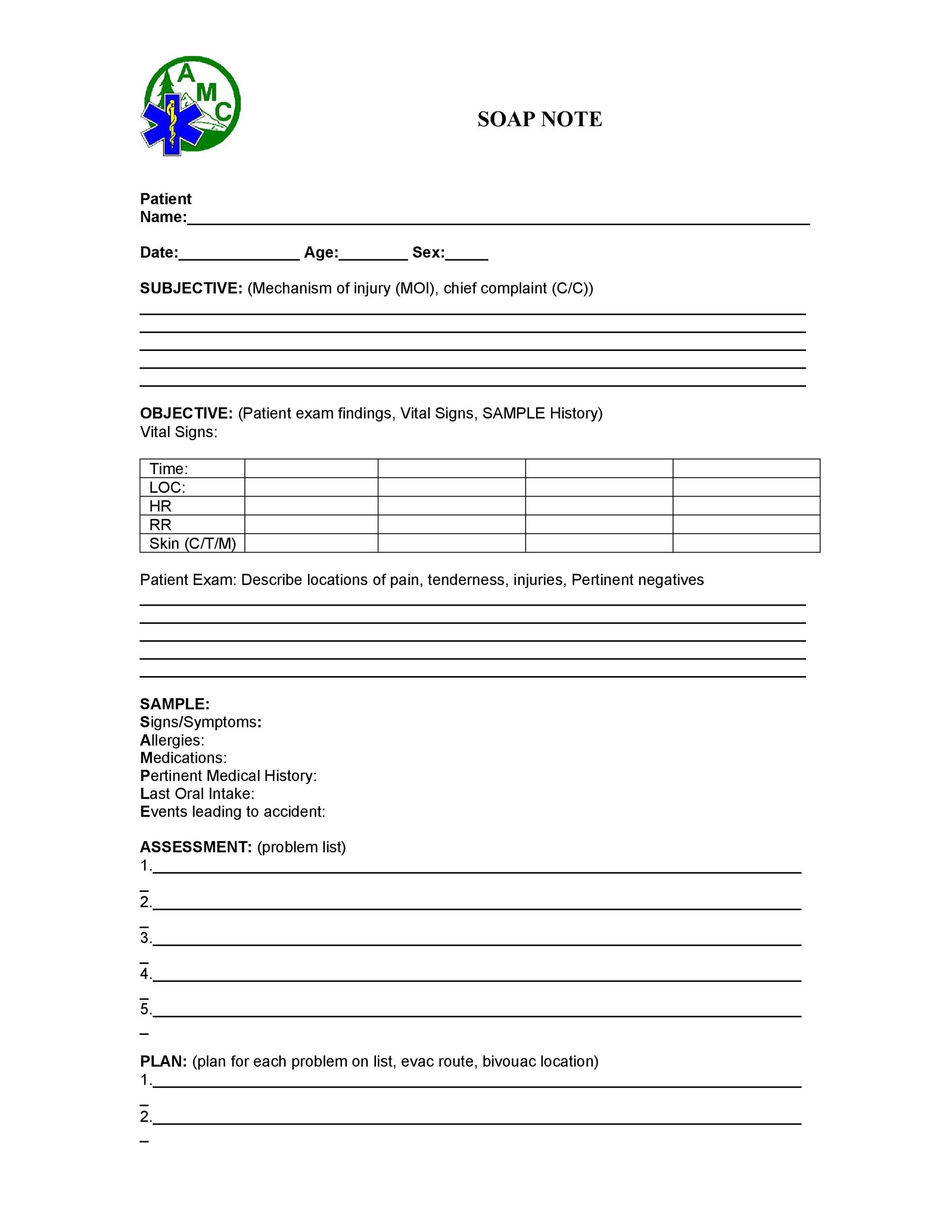
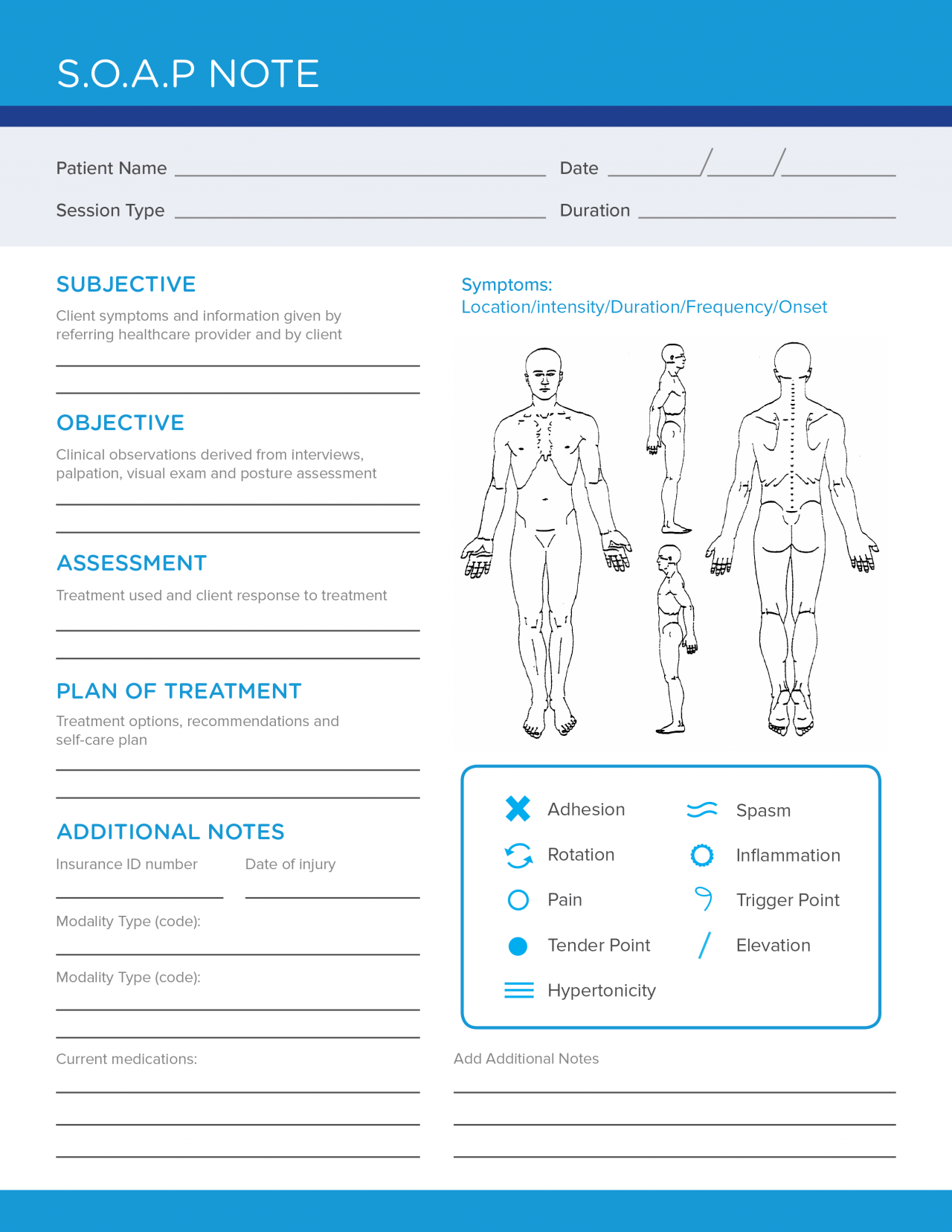
S.o.a.p meaning medical-Subjective includesonset, location, duration;character or symptoms;alleviating/aggravating factors; A SOAP note, or a subjective, objective, assessment, and plan note, contains information about a patient that can be passed on to other healthcare professionals To write a SOAP note, start with a section that outlines the patient's symptoms and medical history, which will be the subjective portion of the note




Proper Hand Washing Visual Guide And Tips
Sample SOAP Note For Social Workers Whether you are a licensed clinical social worker or an MSW social worker, if you have a case load, chances are you need to write case notes also referred to as progress notes If you are required to write your case notes in SOAP note format this post will give you an example of some of the most important thomas7331 SOAP is just a format that some providers use for documenting their encounters It does not change how you code you should still code the encounter based on the content of the documentation, not the format Typically, the S/subjective has the history, O/objective has the exam, and the AP/Assessment & Plan contains the MDM, but notSymbolic Optimal Assembly Program (programming language for the IBM 650 computer in the late 1950's) SOAP Spectrometric Oil Analysis Program SOAP Small Operator Assistance Program SOAP Satellite Orbit Analysis Program (standard program
S O A P NOTE S = Subjective or summary statement by the client Usually, this is a direct quote The statement chosen should capture the theme of the session 1 If adding your own explanatory information, place within brackets to make it clear that it is not a direct quoteBY Matt Soniak iStock A lot of people think that the distress signal is an abbreviationSOAPIE An acronym for a charting mnemonic S ubjective, O bjective, A ssessment, P lan, I mplementation, E valuation
Looking for the definition of SOAPER?Common Medical Abbreviations A AAROM Active assistive range of motion ABG Arterial blood gas ac before meals A/C Assist Control add Adduction ADA Diet American Diabetes Association Diet ADL activities of daily living AFib arterial fibrillation AKA Above Knee Amputation or above the knee amputation ALS amyotrophic lateral sclerosisList of 12 best SOP meaning forms based on popularity Most common SOP abbreviation full forms updated in July 21




Free Soap Notes Templates For Busy Healthcare Professionals




More Medicine Less Wellness
The SOAP Note Template is a documentation method used by medical practitioners to assess a patient's condition It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information Call your doctor for medical advice about side effects You may report side effects to FDA at 1800FDA10 FML SOP side effects (more detail) What other drugs will affect FML SOP? Small animal medical diagnosis by Lorenz Paper only Veterinary clinical examination and diagnosis by O M Radostits Paper only See page 70 for SOAP info Medical History and Physical Examination in Companion Animals by Rijnberk Ebook and Paper See page 40 for SOAP info Last Updated 852 AM;



Gastroenteritis Stomach Flu Instructions Because Gastroenteritis Is




Soap And Detergent Chemistry Uses Properties Facts Britannica
SOAP is listed in the World's largest and most authoritative dictionary database of abbreviations and acronyms SOAP What does SOAP stand for? Soapie charting is S (Subjective data) chief complaint or other information the patient or family members tell you O (Objective data) factual, measurable data, such as observable signs and symptoms, vital signs, or test values A (Assessment data) conclusions based on subjective and objective data and formulated as patient'Standard Operating Procedure' is one option get in to view more @ The Web's largest and most authoritative acronyms and abbreviations resource



Soap Note And Documentation Templates Examples Seniors Flourish




Soap Notes Youtube
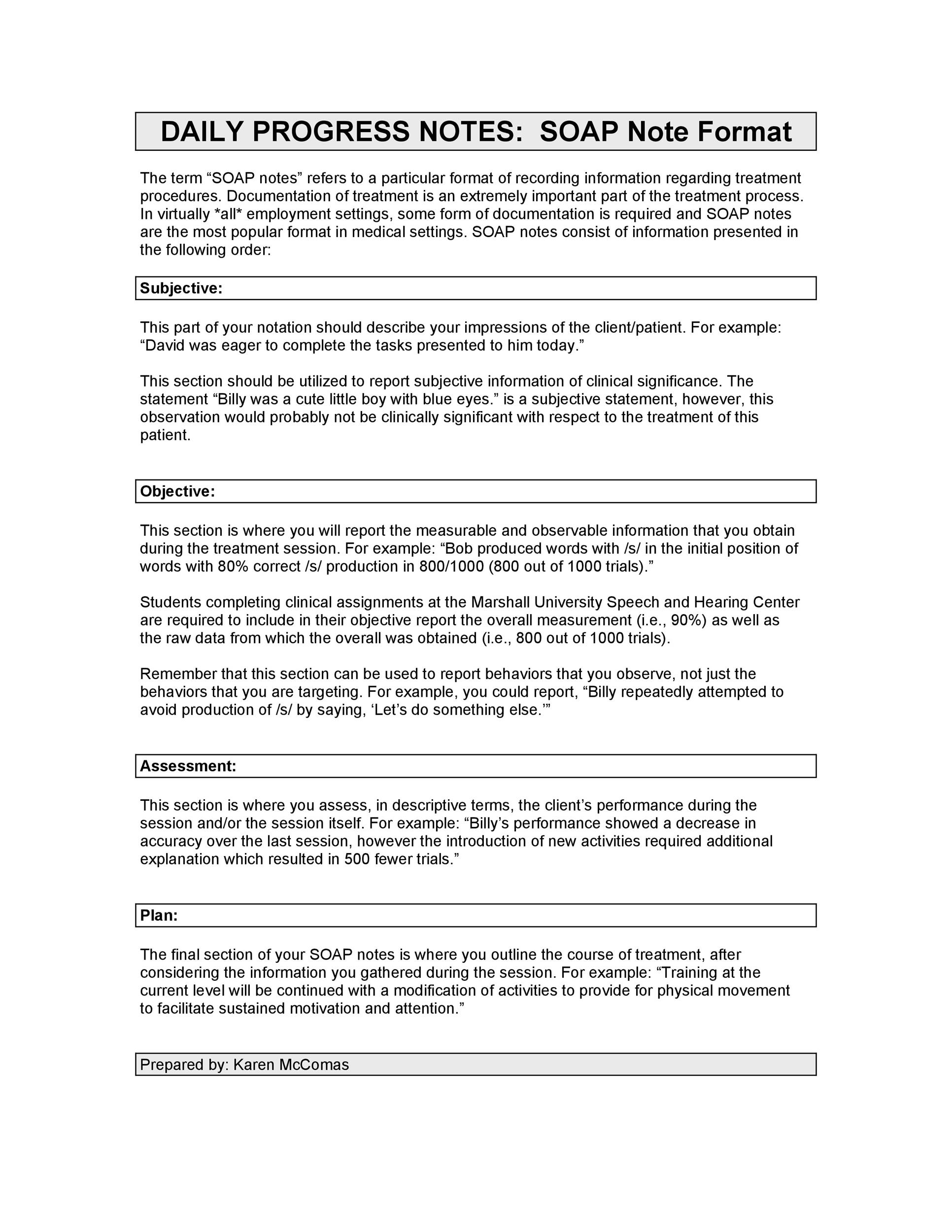
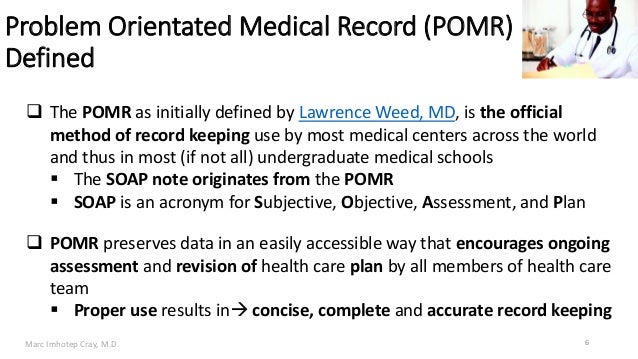
The term "SOAP" simply refers to the 4 headings in this type of report Subjective, Objective, Assessment and Plan= SOAP The basic rule of a SOAP note is brevity; Creating a record of detailed treatment notes allows a medical professional to build their own miniresearch library You will note what works, what doesn't and everything in between Writing great Physical Therapist SOAP notes is a tried and true method for collecting data This data provides reference points throughout a patient's journeyThe Problem Oriented Medical Record and the "Academic" SOAP The goals of the Problem Oriented Medical Record (POMR) The POMR is an instructional tool for teaching both medicine and clinical problem solving skills It is also a useful template for writing medical records for any case that has more than one major problem




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice
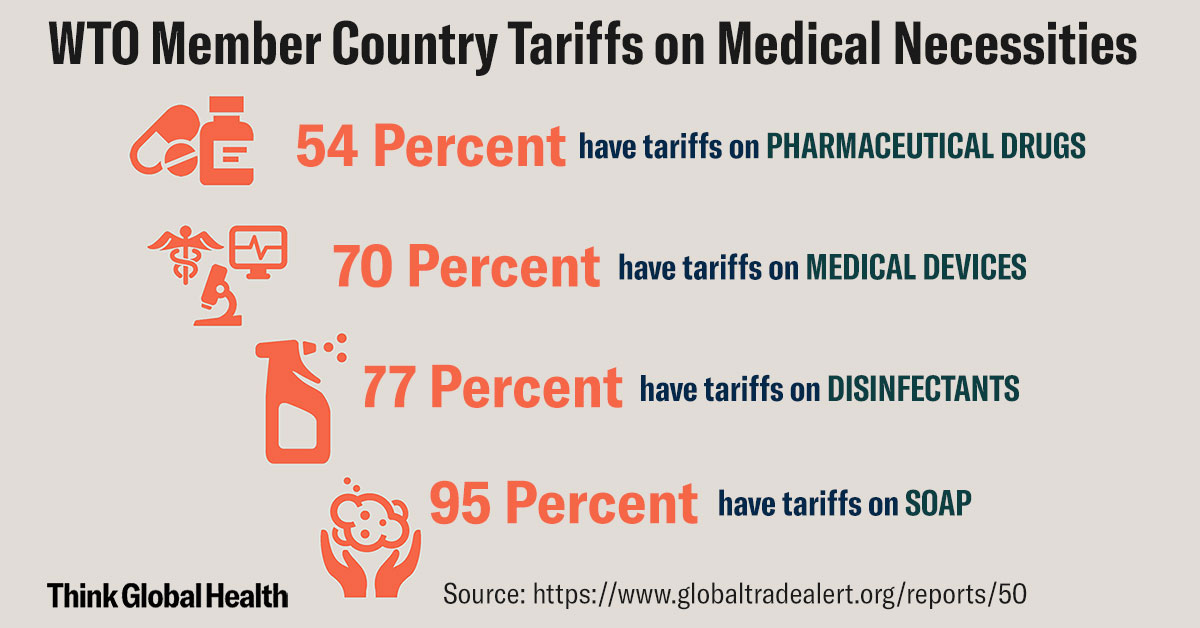



Six Proactive Steps In A Smart Trade Approach To Fighting Covid 19 Think Global Health
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records They allow providers to record and share information The acronym SOAP stands for Subjective, Objective, Assessment, and Plan Each category is described below S = Subjective or symptoms and reflects the history and interval history of the condition The patient's presenting complaints should be described in some detail in the notes of each and every office visitMedicine used in the eyes is not likely to be affected by other drugs you use But many drugs can interact with each other




Understanding Soap Format For Clinical Rounds Global Pre Meds




Planning Patient Care Healthcare Service Delivery
What does SOAP abbreviation stand for?Temporal pattern(time of day, all day);associated symptoms Objective vital signsThe SOAP note stands for Subjective, Objective, Assessment, and Plan This note is widely used in medical industry Doctors and nurses use SOAP note to document and record the patient's condition and status The SOAP note is considered as the most effective and standard documentation used in the medical industry along with the progress note



40 Fantastic Soap Note Examples Templates ᐅ Templatelab




Hcm210 Medical Terminology Soap Notes Youtube
This is not usually a lengthy history detailing all the facts of the patient's health statusMiami Dade College Medical Center Campus Emergency Medical Technician SSOAP OAP RReport eport FFormatormat (S)ubjective In this area you will document anything that the patient or family & friends tell youLooking for online definition of SOAP or what SOAP stands for?




Tips For Writing Better Mental Health Soap Notes Updated 21




The Evolution Of Office Notes And The Emr The Caps Note Consult Qd
There are four components that form these notes that make up the acronym SOAP S is for subjective , or what the patients say about 2 SOAP note for counseling sessions (PDF) 3 SOAP note for coaching sessions (PDF) A TakeHome Message Whether you are in the medical, therapy, counseling, or coaching profession, SOAP notes are an excellent way to document interactions with patients or clientsSOAP notes are easy to use and designed to communicate the most relevant information about theFind out what is the full meaning of SOP on Abbreviationscom!



Www Wto Org English News E News E Rese 03apr E Pdf




What Are Soap Notes In Counseling Examples
Signs You Need Relief From Chronic Pain Syndrome (CPS) There are no medical instruments to measure pain It affects people differently, and doctors typically rely on a patient's own description of their CPS before recommending pain management treatments The START acronym is a specific system set up for EMS to triage a scene with a large number of patients The START system is designed to be a very rapid assessment that categorizes treatment priority of patients in under a minute for rescuersThese are flagged in the list of abbreviations used in medical prescriptions Orthographic styling Periods (stops) Periods (stops) are often used in styling abbreviations Prevalent practice in medicine today is



1
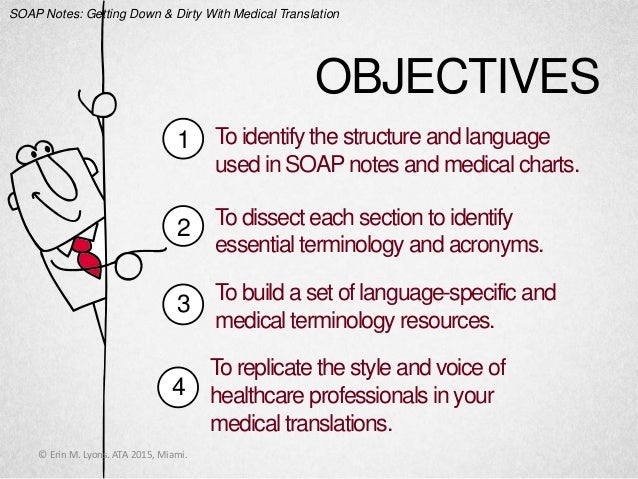



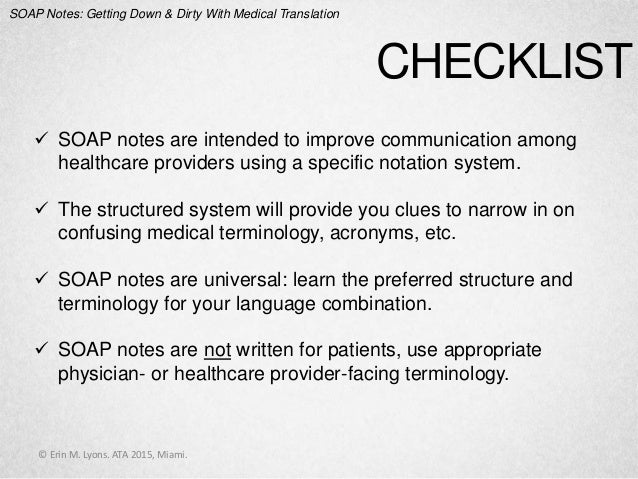
Soap Notes Getting Down And Dirty With Medical Translation
List of 3 best SOAP meaning forms based on popularity Most common SOAP abbreviation full forms updated in July 21 The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers The SOAP note is a way for healthcare workers to document in a structured and organized way This widely adopted structural SOAP note was theorized by Larry Weed almost 50 years ago A SOAP note is information about the patient, which is written or presented in a specific order, which includes certain components SOAP notes are used for admission notes, medical histories and other documents in a patient's chart




Coronavirus Questions Answered What We Know About Covid 19 Time




Conceptual Hand Writing Showing Rapid Test Kit Concept Meaning Emergency Medical Diagnostic Equipment That Deliver Fast Results Primary Medical Preca Stock Photo Alamy
What is a SOAP Note – Definition A SOAP note is a document usually used in the medical fraternity to capture a patient's details in the process of treatment This is one of the many formats that are used by professionals in the health sector The SOAP note is usually included in the patient's medical record for the purpose of informingS stands for subjective data provided by the patient, O for objective data gathered by health care professionals in the clinical setting, A for the assessment of the patient's condition, and P for the plan for the patient's careCertain medical abbreviations are avoided to prevent mistakes, according to best practices (and in some cases regulatory requirements);
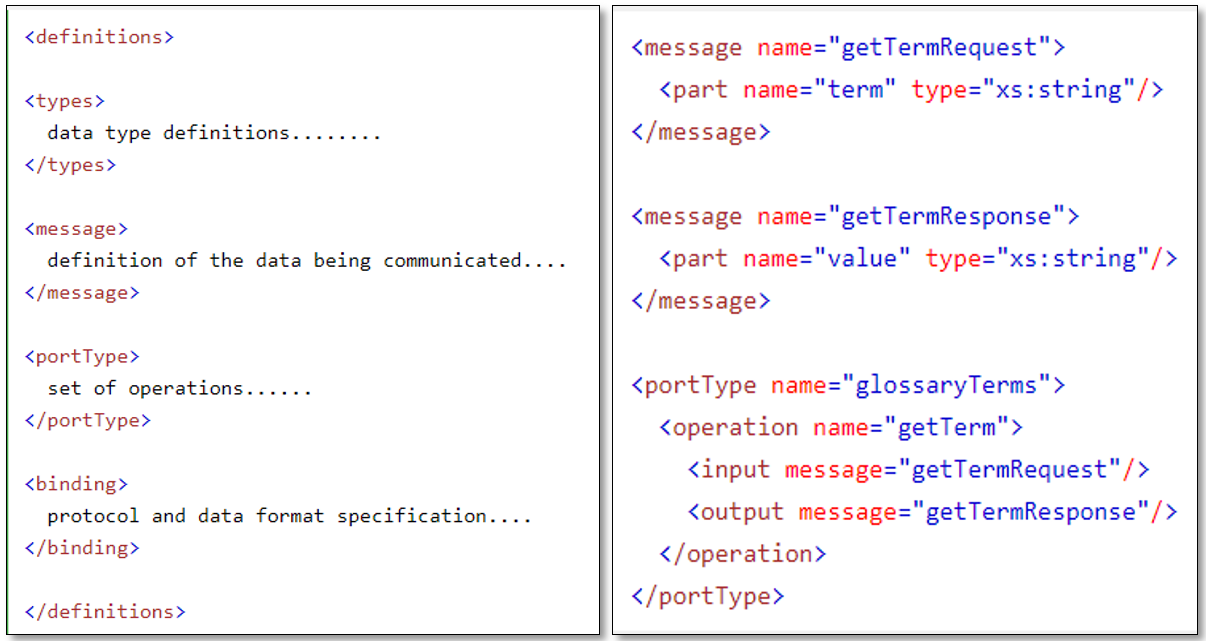



Webservices Soap And Rest A Simple Introduction



Preparing For The Worst No Match Monday The Vocal Cord
was developed for medical and mental healthcare providers in the late 1960s They used SOAP notes to organize symptoms, observations, assessments and the treatment plan The ultimate goal of the system was to improve communication among all medical disciplines caring for a patient "SOAP notes have been used by therapists for decades," says Ann What Does SOS Stand For? SOAP Notes in the Medical Field The SOAP note is an essential method of documentation in the medical field It's imperative that every student learn the basics for writing a SOAP note to become a health care provider like a physician or an Advanced Practice Nurse




How To Write Incredible Physical Therapist Soap Notes
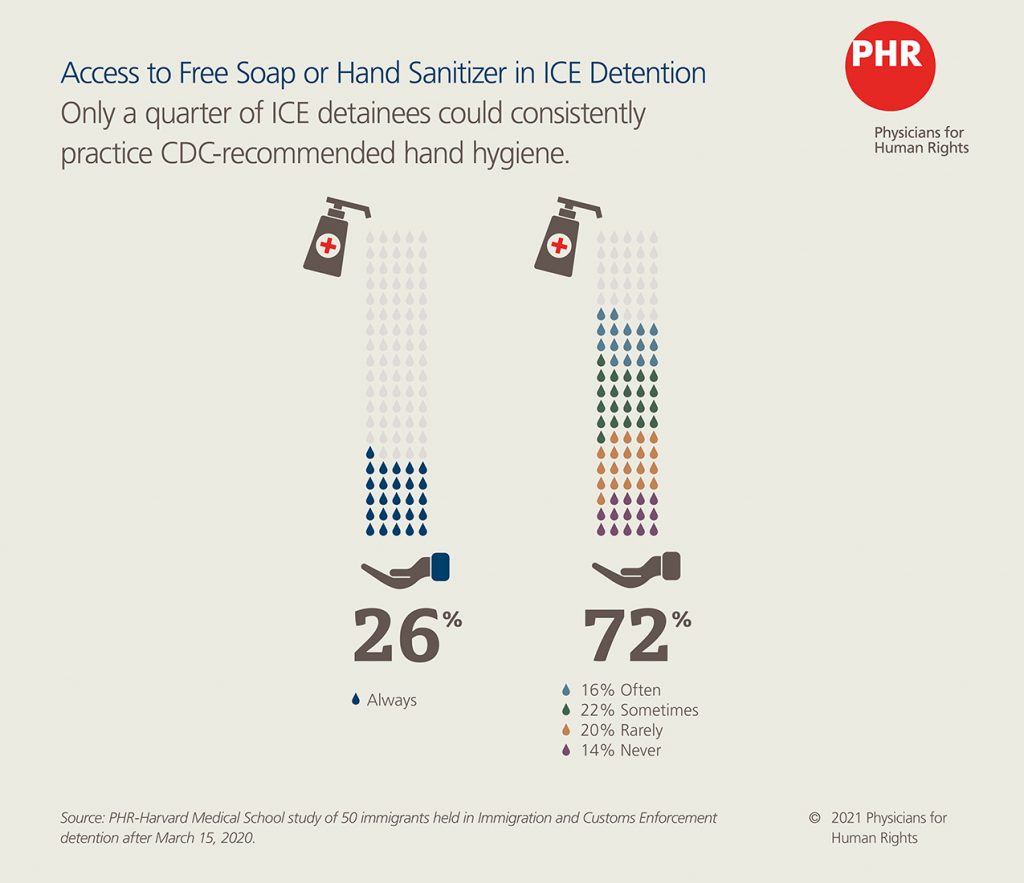



Praying For Hand Soap And Masks Physicians For Human Rights
Why SOAP Notes Are an Important Tool SOAP is the most common format used by medical and behavioral health professionals, and for good reason Since its development in the 1960s, the SOAP framework has been useful enough forLooking for the definition of SOP?'Subjective Objective Assessment Plan Evaluate Reevaluate' is one option get in to view more @ The Web's largest and most authoritative acronyms and




How To Write A Soap Note With Pictures Wikihow
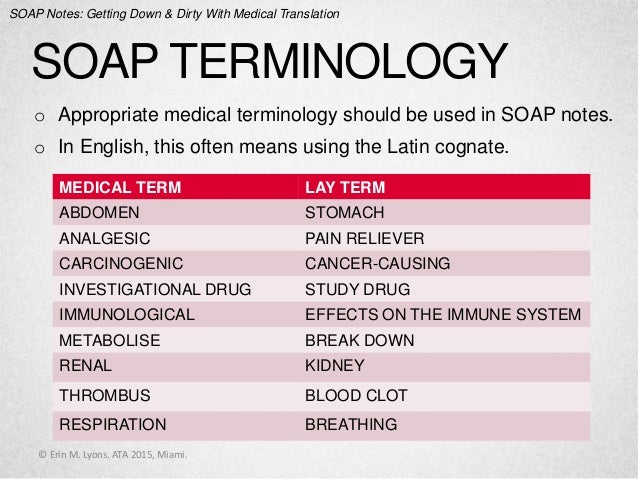



Soap Notes Getting Down And Dirty With Medical Translation
Medical Chart Notes SOAP A chart note usually follows a very simple pattern S ubjective (what the patient thinks) = S O bjective (what the doctor thinks) = O A ssessment (what the diagnosis is) = A P lan (what happens next) = PThe Free Dictionary or advice of a legal, medicalIt's a template for documentation S Subjective a description of the information you received that cannot be proven, specifically measured or independently verified, eg "Nurse I am in pain" O Objective anything that can be measured, observe




What Does Soap Stand For




Free Soap Notes Templates For Busy Healthcare Professionals
Acronym for the conceptual device used by clinicians to organize the progress notes in the problemoriented record;Soap definition is a cleansing and emulsifying agent made usually by action of alkali on fat or fatty acids and consisting essentially of sodium or potassium salts ofSOP Standard Operating Procedure SOP Separation of Powers SOP Sex on Phone




Who S Infection Prevention Control Department




Proper Hand Washing Visual Guide And Tips
What does the O mean in HOPS Compare the non hurt to the injury, look for bleeding, deformity, swelling,discoloration,scars, and other signs of trauma What does the P mean in HOPSThe main purpose of the patient's medical visit is to seek treatment and so the assessment should contain all the symptoms stated by the patient along with the diagnosis of the illness or injury It should also include a differential diagnosis or a list of other likely findings, arranged in order of the most likely one to the least likely one All the slick Web pages, billboards, telephone marketers, direct mailings and open houses cannot compete with the most important clinical tool—SOAP, which stands for Subjective observation, Objective observation, Assessment and Plan A complete individual patient assessment should be performed consistently at every visit How to use SOAP



Medical Mnemonics Diagnostic Criteria For Sle Soap Brain Md Usmle Internal Medicine Abim Board Exam Review Blog



Cuticura Soap Wikipedia



Fcm Unm Edu Education Images Docs Template Clin Soap Note Pdf



Nutritional Progress Notes Ppt Video Online Download



Http Www Trekds Com Techinfo Msds Files Sen Ecsds Cation adjusted mueller hinton broth w lysed horse blood v1 3 Pdf



Www Nrmp Org Wp Content Uploads 15 09 Soap Faq Schools Pdf




Conceptual Hand Writing Showing Medical Checkup Concept Meaning The Examination Carried Out To Determine The Physical Fitness Primary Medical Precaut Stock Photo Alamy



Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



Pomr And Soap Notes



2




Medical Terminology And Abbrev Pages 1 10 Flip Pdf Download Fliphtml5




Focusing On Health Laboratory Exercises In Microbiology Bluedoor Publishing




What Is Chlorhexidine Soap With Pictures



What Does S O A P Mean Definition Of S O A P S O A P Stands For Subjective Objective Assessment Plan By Acronymsandslang Com




4 Common Mistakes To Avoid When Writing Soap Notes Simplepractice



2




Medical Archives Emottawa Blog




Soap Notes Resources Digital Chalkboard




Free Soap Notes Templates For Busy Healthcare Professionals



2




What Does Soap Mean Soap Definitions Abbreviation Finder




Say Goodbye To Antibacterial Soaps Why The Fda Is Banning A Household Item Science In The News




How Soap Notes Paved Way For Modern Medical Documentation




Free Soap Notes Templates For Busy Healthcare Professionals




Lifebuoy Soap Vintage Advertising Art Vintage Medical Vintage Ads




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software




The Soap Opera And Its Affect On Media Culture And Society Mr Hughes Ppt Download



Free 15 Soap Note Templates In Pdf Ms Word



Praying For Hand Soap And Masks Physicians For Human Rights



1




Stay Safe Medical Block Sogam Facebook




How To Write Incredible Physical Therapist Soap Notes



Tips For Writing Better Mental Health Soap Notes Updated 21



40 Fantastic Soap Note Examples Templates ᐅ Templatelab
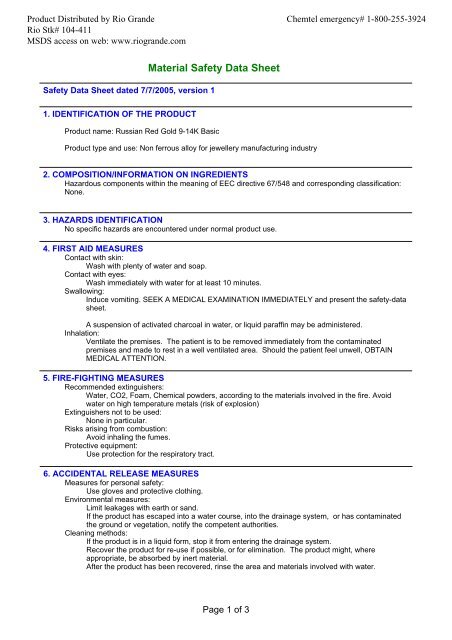



Russian Red Gold 9 14k Basic Msds Rio Grande



Www Nmhealth Org Publication View Help 4634




Soap Note How To Write Spotless Healthcare Notes Free Template Process Street Checklist Workflow And Sop Software



Webservices Soap And Rest A Simple Introduction




Say Goodbye To Antibacterial Soaps Why The Fda Is Banning A Household Item Science In The News
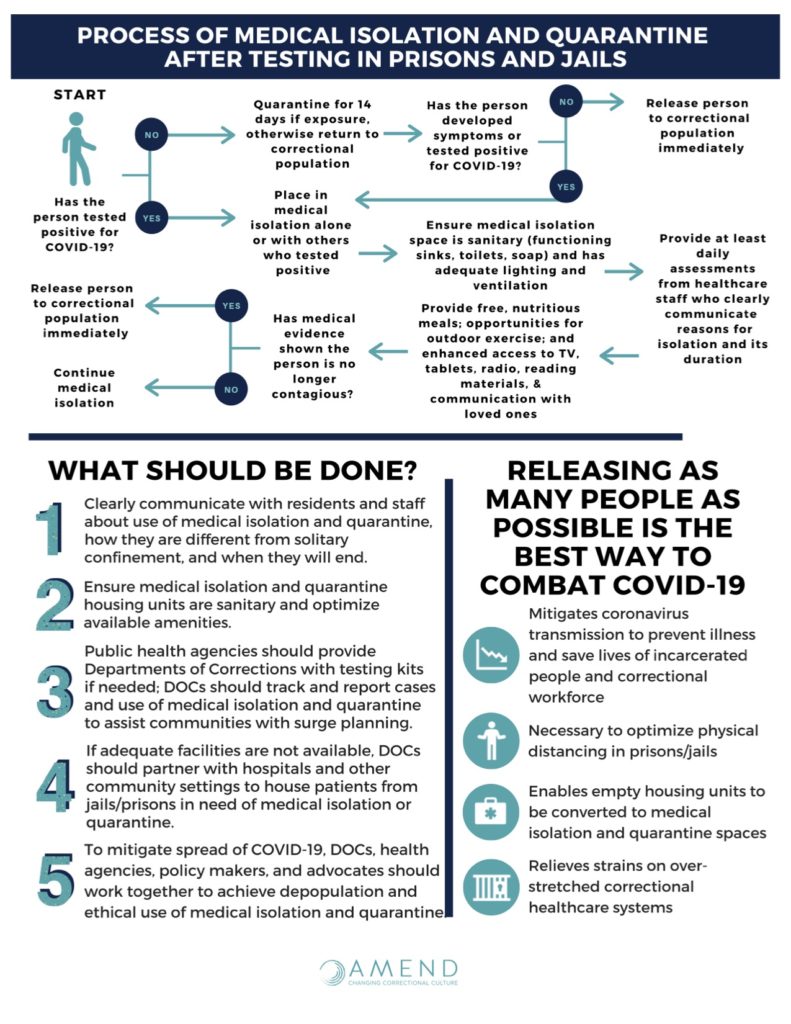



Covid 19 In Correctional Facilities Medical Isolation Amend



Soap Subjective Objective Assessment Plan By Acronymsandslang Com




Antibacterial Soap Vs Regular Soap Which One Is Better




Top 5 Skin Benefits Of Activated Charcoal Soap For Face




Mild Soap What You Need To Know About Its Benefits And Uses



Medical Terminology Learning Terminology Ppt Video Online Download




Hand Hygiene And Handwashing Nurseslabs



Soap Subjective Objective Action And Plan Of Treatment By Acronymsandslang Com
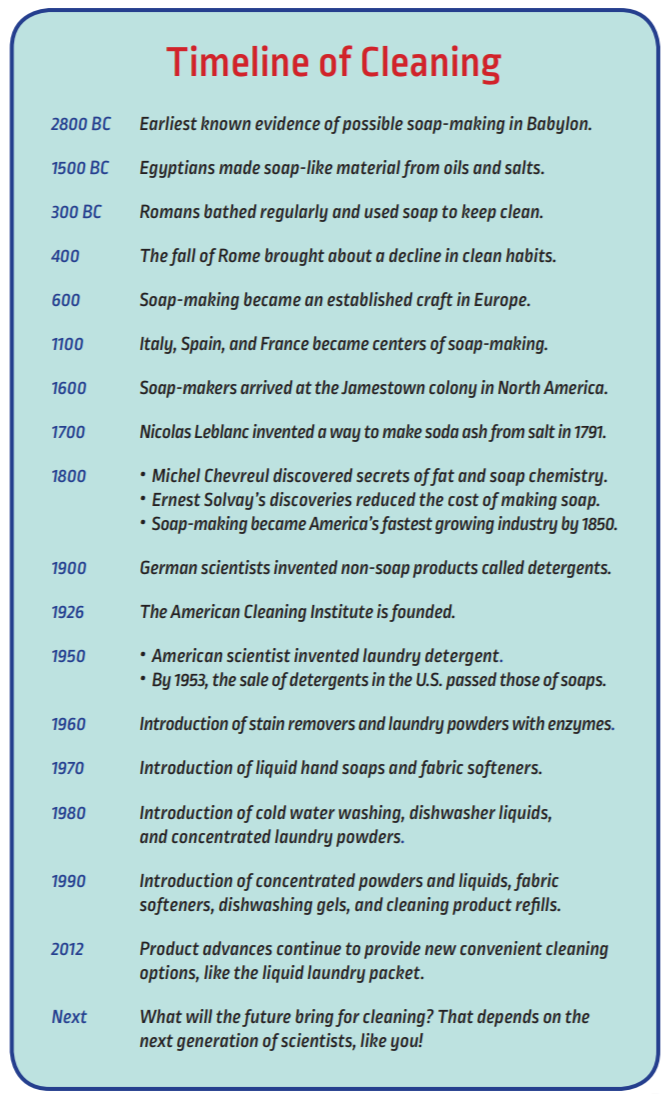



Soaps Detergents History The American Cleaning Institute Aci
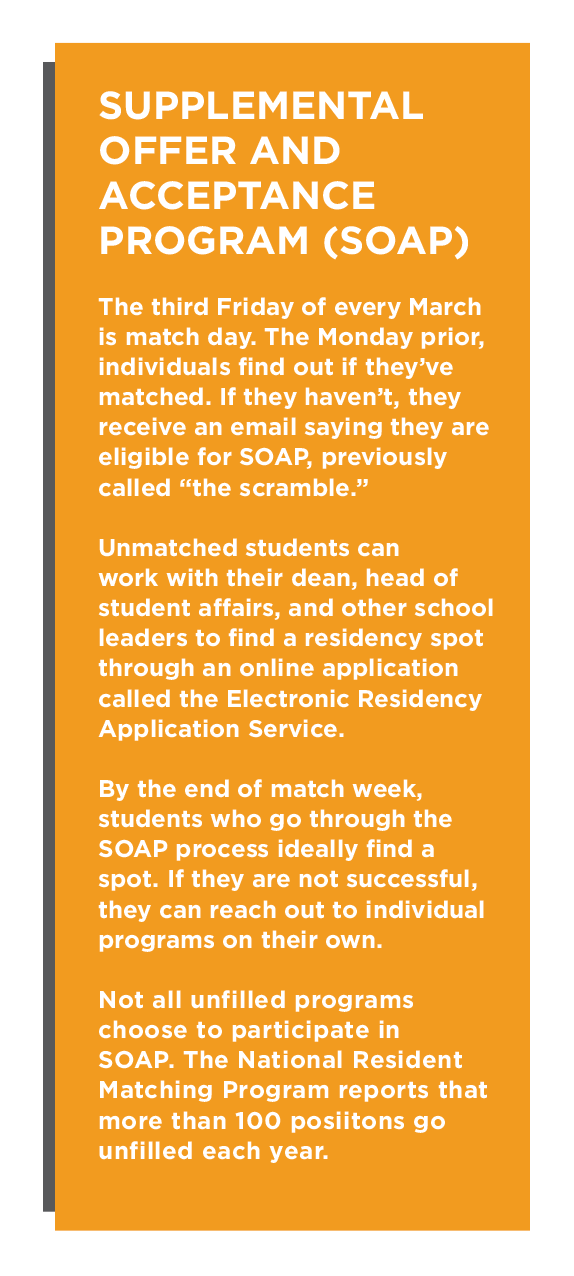



Healthcare Suffers When Medical School Graduates Don T Match Insight Into Diversity



Progress Notes



Www Homestatehealth Com Content Dam Centene Home State Health Pdfs Meat Documentation Tips Pdf



1



Patient Soap Note Charting Procedures



How To Document A Patient Assessment Soap Geeky Medics




51 Sample Soap Notes In Pdf Ms Word Excel



Tips For Writing Better Mental Health Soap Notes Updated 21



1




Soap Notes The St John S Pa Program Survival Guide



2



Using Medical Note Taking Skills On Teaching Journal Kwarrior Eng Clinic




Soap Note



2




What Are Problem Oriented Medical Records True North Itg



40 Fantastic Soap Note Examples Templates ᐅ Templatelab
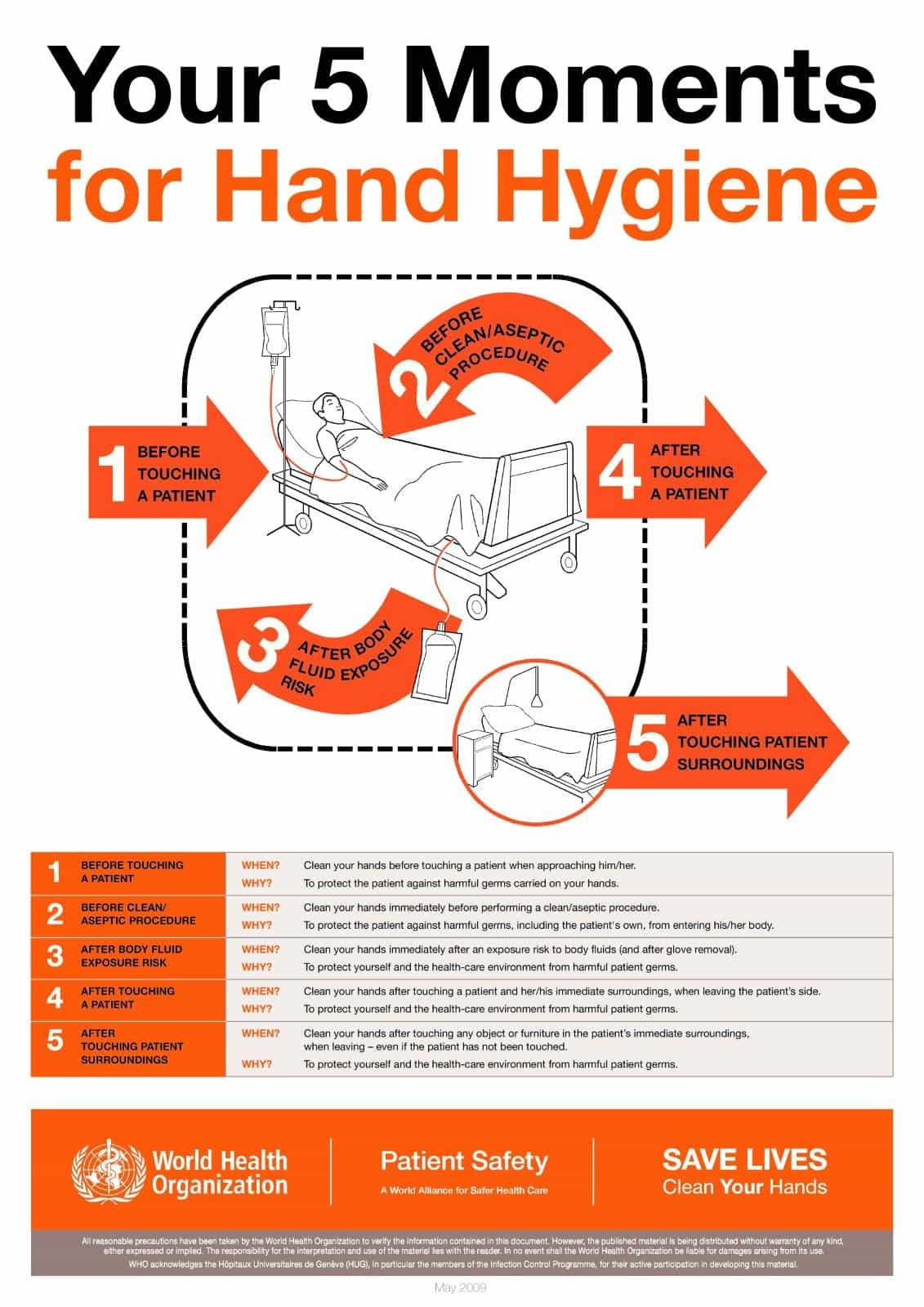



Hand Hygiene And Handwashing Nurseslabs



Http Www Ravenwood Pa Com Npceu Fdu 6680 Doc 6680 7728 F02 Guide Shp Pdf




Handwriting Text Writing Ask Your Doctor Concept Meaning Seeking Information Or Advice From A Medical Professional Canstock




What Is A Soap Note Jess Brantner Wvu Dietetic Intern



What Are Soap Notes In Counseling Examples



Leptospirosis Treatment Symptoms And Types
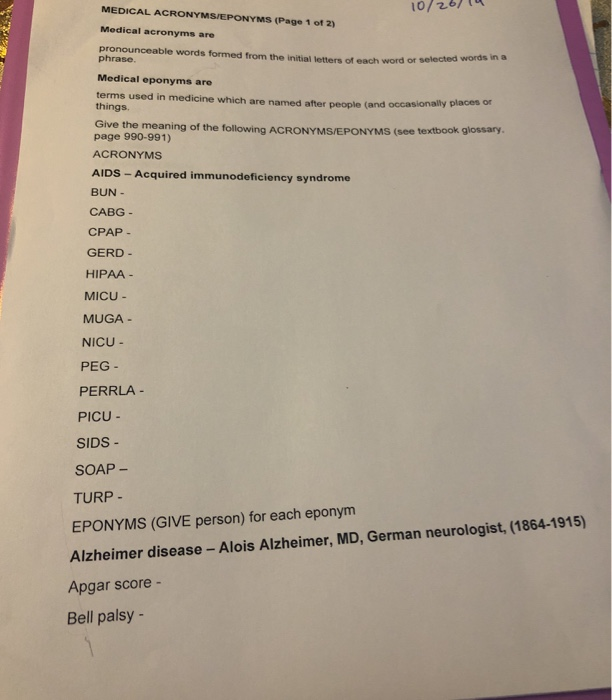



10 Medical Acronyms Eponyms Page 1 Of 2 Medical Chegg Com




Hand Washing Wikipedia



Soap Notes Getting Down And Dirty With Medical Translation
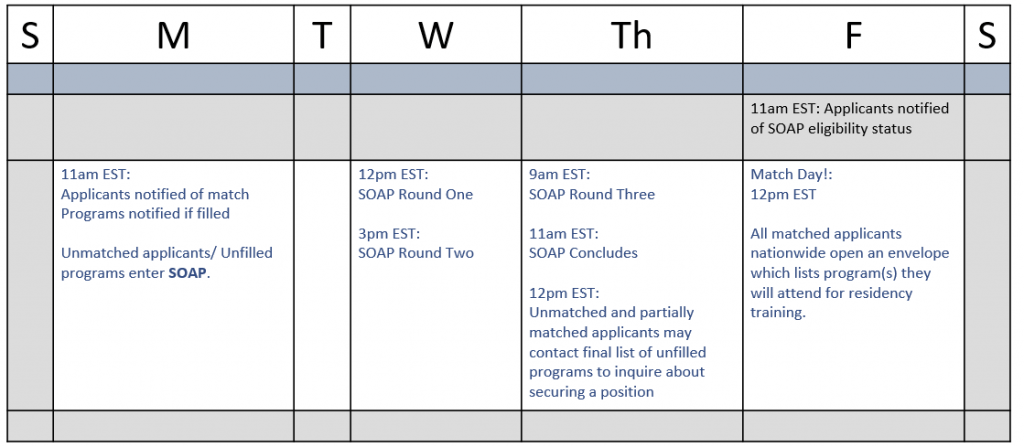



The Ultimate Guide To The Medical Residency Match Process Thalamus



0 件のコメント:
コメントを投稿